Pam Belluck, who covers maternal mental health, visited and talked with women across the country who experienced postpartum depression.
Depression descended on Samantha Cohn about two months after her baby boy was born.
He was thriving, but she became convinced she was a terrible mother. "I felt like I wasn't doing enough, I wasn't doing anything right," she said. She began to think her son and husband might be better off without her. When the baby was about 5 months old, she tried to take her life with a gun.
Ms. Cohn, 30, who lives near Fayetteville, N.C., was hospitalized for weeks and underwent surgeries to repair damage to her jaw, nose, tongue and face. But her postpartum depression remained challenging to treat. The hospital's maternal mental health specialists decided to have her try a medication that had recently become available: the first pill specifically for postpartum depression.
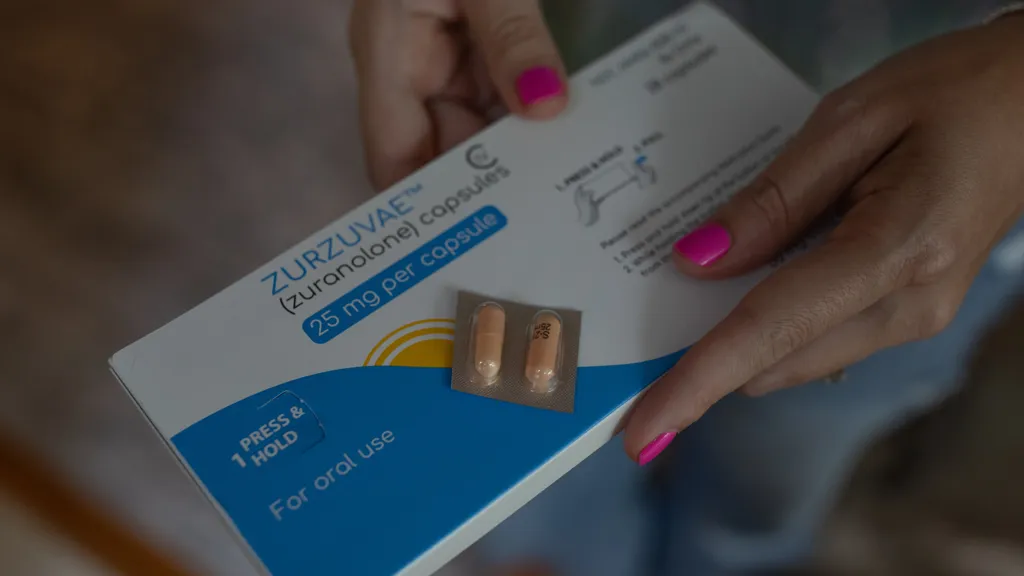
Clinical trials had found that the drug, zuranolone, marketed as Zurzuvae and taken daily for 14 days, can ease symptoms for some women in as little as three days, while general antidepressants can take weeks. For Ms. Cohn, its impact was swift and striking. On her fourth day of taking it, she said she suddenly "felt so much clarity in my head, like I didn't have nagging thoughts about not being good enough."
Now, a year and a half after the drug became available, thousands of women have tried it, and their experiences have run the gamut. For some, symptoms improved remarkably. Others described a modest benefit that didn't last or said their depression persisted. And others didn't complete the two-week regimen because profound drowsiness, a common side effect of the drug, interfered with their ability to care for their babies or to fulfill other responsibilities.
One in eight women in the United States experiences depression during pregnancy or in the year after giving birth, the Centers for Disease Control and Prevention estimates, and effective treatments are crucially needed. While the fast-acting pill shows promise, doctors say the challenge now is to determine which patients will benefit and why some don't.
Clinical trials of the drug found that postpartum depression improved in about 60 percent of patients. "It's not everyone," Dr. Samantha Meltzer-Brody, a leader of the trials and director of the Center for Women's Mood Disorders at the University of North Carolina at Chapel Hill, said at a National Institutes of Health conference. "So, what is it about the people that are going to respond versus those that don't?"
Stacey, 42, of San Diego, who asked to be identified by her first name to protect her privacy, said Zurzuvae made her "so tired" that after several days of taking it, "I just felt like a zombie."
"I actually felt more depressed while I was on it," she said.
To address Stacey's response to the medication, Dr. Alison Reminick, director of women's reproductive mental health at the University of California, San Diego, advised her to take half doses for the rest of the 14 days. But Stacey said she stopped Zurzuvae altogether, halfway through the regimen, because the sluggishness made it difficult to care for her baby.
"The medication is incredibly sedating," Dr. Reminick said. "There's a warning on the box. They can't drive for 12 hours after taking it and they can't really take care of their children without help."
Yet, some patients don't experience sedation and others welcome it because it helps them get much-needed sleep and feel less overwhelmed, said doctors who prescribe Zurzuvae.
The week after Ms. Cohn started taking Zurzuvae, the turnaround of her symptoms was so obvious that she was discharged from the hospital. "She had a really nice improvement of her postpartum depression with that medicine," said Dr. Riah Patterson, a psychiatrist at U.N.C. Chapel Hill.
Ms. Cohn finished the 14-day regimen at home and attended intensive outpatient therapy for months. Now, she has gone back to work as a tattoo artist, and she said that with weekly therapy and an anxiety medication, she is managing the aftermath of the crisis, including undergoing additional surgeries.
"I'm just excited to get a little bit closer to really being me again," she said.
She no longer feels anxious about her parenting ability and enjoys playing with her son and taking him to places like the local children's museum. "He makes everything worth pushing through."
Importance of quick intervention
Zurzuvae is a synthetic version of a steroid called allopregnanolone that originates in the brain. The theory behind the medication is that perinatal depression often arises as hormones that surge in pregnancy plummet during childbirth. Some women seem particularly sensitive to that sudden drop-off, which also lowers levels of the steroid, Dr. Meltzer-Brody said.
Zurzuvae can be taken with other antidepressants and since it is prescribed for only a single 14-day course some doctors use it as an adjunct or bridge to ease severe symptoms before longer-term use of antidepressants.
Some patients who are breastfeeding have declined to take the drug because its penetration of breast milk has not yet been studied. Doctors said it is likely safe but if patients are concerned they might pump two weeks’ worth of milk before starting Zurzuvae.
Initial logistical hurdles in obtaining Zurzuvae frustrated doctors who said the delays undermined the purpose of a quick-acting medication. Some insurers initially set strict conditions for covering the drug which has a list price of $15,900. Doctors said some insurers required patients to try other antidepressants first or to obtain prescriptions from psychiatrists—steps that went beyond the F.D.A. requirements for Zurzuvae.
Joy Burkhard chief executive of the Policy Center for Maternal Mental Health said most insurers and Medicaid no longer have such barriers but a few still require extra steps.
Zurzuvae is not available in retail pharmacies only specialty pharmacies that require patients to take various measures to validate insurance and delivery information according to a spokeswoman for the drug's manufacturer Sage Therapeutics which markets Zurzuvae in partnership with Biogen.
Chris Benecchi the chief operating officer of Sage which is expected to be acquired by Supernus Pharmaceuticals later this year said Sage had worked to resolve logistical issues and prescriptions had increased.More than 10,000 orders have been sent to patients so far Sage said adding that about 80 percent of the prescriptions were issued by obstetrician-gynecologists.
"The majority of patients are able to get the medication within days," Mr. Benecchi said, adding that if patients encounter delays,Sage will ship Zurzuvae directly "as rapidly as possible."
Quick access is crucial doctors say.Hannah Ginther was hospitalized for a week last summer at U.N.C.Chapel Hill for symptoms that included obsessively worrying that her second child,then 10 months old,had a neurological disorder,ealthough doctors said the baby did not.
"I just couldn't get out of that loop of jumping to worst-case-scenario," Ms.Ginther,36,say at her home in Wilmington,N.C."I would throw up.I struggled to get out of bed,struggled to do basic,daily-living things."
When she was discharged from the hospital,dctors prescribed Zurzuvae,but her insurance rejected coverage,saying she would qualify only if she had developed postpartum depression in her last trimester of pregnancy,or within four weeks after childbirth,Dr.Pattersonsaid.Ultimately,the hospital appealed to Sage,whichsent the drug to Ms.Ginther at no cost.
But the insurance hiccups had caused a two-week delay,during which,Ms.Ginthersaid,hersymptoms“spiraled again.”She was rehospitalized for nine days.Dr.Riddle,a psychiatrist at U.N.C.Chapel Hill,saidthe second hospitalization might have been avoided if the Zurzuvae had arrived sooner.
By the time it reached Ms.Ginther,she had been stabilized with other medications and intensive therapy.She said Zurzuvae didn't add much,except possibly further improving her mood and sleep.
"I think if we had been able to have access to Zurzuvae sooner,it would have shortened some of the pain,but they were able to find other medications that helped me," Ms.Ginther said.
She has since reduced her workload and continues taking Prozac.She has no intrusive thoughts and is "doing much better," she said.
Effective for some,but not all
As doctors try to determine which patients Zurzuvae can help,Jenny Sharma's experience illustrates the complexity.Ms.Sharma,43,of San Diego,had a history of depression,especially linkedto menstruation,but it was not as severe as the depression she experienced after giving birth in August 2023.Several months later,she began feeling suicidal and she said she also had "homicidal thoughts toward the baby," vivid and terrifying images.
She sought help from Dr.Reminick's program,trying different medicationsover several months.While taking Zurzuvae,her symptoms improved."I felt wonderful," she said.
Dr.Reminick said Ms.Sharma’s response to Zurzuvae was “the best I’ve ever seen her.”But,she said,about 11 days intothe 14-day regimen,Ms.Sharma startedspeaking haltingly and appeared to have “cognitive difficulties,whole body shakingand twitching,confusionand dizziness.”
Dr.Reminick said it was unclear whether those symptoms were linked to Zurzuvae or to another medication.Overall,she said she considered Zurzuvae a “good fit” for Ms.Sharma,but her improvement didn’t last.
"About a month later,my symptoms all came raging back," Ms.Sharma said."Afraid that I would harm my baby,I visited an emergency room and then had several psychiatric hospitalizations and electroconvulsive therapy.Eventually,with other medications and some supplements,my mental health stabilized although I occasionally experience brief periods of depressive thoughts,"she said.
In clinical trials,patients helped by Zurzuvae continued doing well 45 days later.About half of those who took Zurzuvae were considered to be in remission.Dr.Riddle is following patients to see if the benefit can last longer.
"No one's illness is exactly the same," Dr.Riddle said.So far "no one has said they'd never take it again;it's just varying levels of how helpful it was."
For Kara Fiscus,37,of Sacramento,the benefit has lasted more than a year.Her depression began about five months after her son was born in May 2023.She felt so overwhelmed that she wrote in her journal,“I should kill myself.”
Ms.Fiscus,a former N.F.L.cheerleader,said she had been prepared for some depression because she had mental health challenges in her teens and 20s.But her postpartum symptoms—especially anxiety over not producing enough breast milk and about her baby’s weight—were worse than anything she had experienced.
“When you have a child and you’re not able to meet their needs,it’s no longer that your life is not meeting your own standards—you feel like an impediment to other people,”she said.
Her obstetrician,Dr.Hailey MacNear,prescribed Zoloft and,when that didn’t work,Prozac.But before enough time had passed to know whether Prozac could help,Ms.Fiscusbegan planning to take her own life.
After calling Dr.MacNear,she entered a partial hospitalization program followed by intensive outpatient treatment,but continued thinking of ending her life.
Then,Dr.MacNearprescribed Zurzuvae,which had just become available.On the third day,Ms.Fiscusrealized,“‘Oh my god,I haven’t thought about killing myself in at least 20 minutes.’”And “by Day 7,I was feeling really,really great.”
Dr.MacNearsaid that not every patient experienced similar improvement and that some declined to try it because of the sedative effects.But she saidMs.Fiscuscalled her and “cried with relief” after taking it.
While taking Zurzuvae,Ms.Fiscuscontinued breastfeeding and returned to work,eventually becoming an official at a nonprofit.She still takes Prozac,but credits Zurzuvae with ending her thoughts of self-harm.She even saved the box.
"It's a comfort seeing it," she said."There's hope in that box."