Obesity is a known risk factor for many diseases, but new research now suggests that where on the body fat is stored is even more critical than the number on the scale.
Researchers in the UK's Integrative Cancer Epidemiology Programme (ICEP) in Bristol examined whether body fat distribution affects the risk of 12 cancers, including endometrial (of the uterus), ovarian, breast, colorectal and liver cancer.
They found that the presence of fat around the organs was a significant risk factor, and the relationship between fat distribution and cancer risk varied by cancer type.
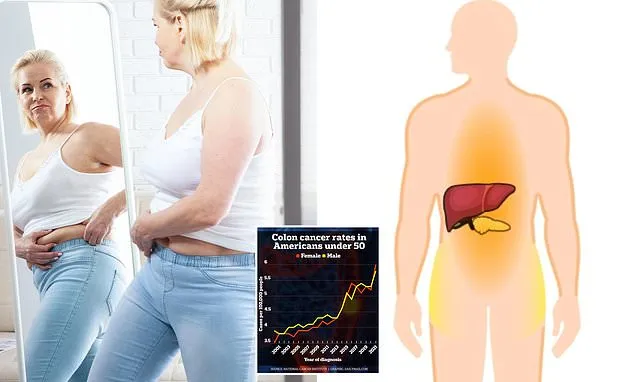
Deep invisible abdominal 'visceral' fat and fat around the liver and pancreas were linked to higher risks of various cancers, including liver, ovarian and thyroid.
Fat stored subcutaneously, the type people generally think of because it is visible, or fat below the waist, showed a more complex relationship, at times raising the risk, while other times being protective.
Dr Emma Hazelwood, lead author of the study, said in a statement: 'These findings support the growing consensus that BMI [body mass index], while useful for population-level trends, may be too simplistic for assessing individual health risks.'
'It is vital to understand the biological mechanisms that underpin these associations, particularly how and why different fat depots affect cancer development.'
BMI, calculated by dividing a person's weight in kilograms by the square of their height in meters, is an outdated health metric because it fails to distinguish between dangerous visceral fat and less harmful subcutaneous fat.
Additionally, since muscle is denser and weighs more than fat, a very muscular person can be classified as overweight or obese by BMI despite having low body fat.
Visceral fat actively drives cancer risk by creating a state of chronic inflammation and hormonal imbalance.
Deep abdominal fat functions like an active organ, producing hormones and inflammatory proteins, rather than merely serving as inert storage.
This activity can damage DNA and promote the growth of tumors.
Its location allows it to flood the liver with these substances, contributing to fatty liver disease, diabetes and other metabolic disorders.
To prove fat storage directly causes cancer, researchers used a genetic technique showing that a predisposition to store fat in certain areas raises risk by altering blood biomarkers like hormones and inflammation.
The strongest links found were that fat inside organs dramatically increases risk.
Liver fat quadrupled the risk of liver cancer, equaling a 309 percent increased risk, and pancreatic fat doubled the risk of endometrioid ovarian cancer.
The link between body fat and cancer is location-specific. Dangerous deep visceral and organ fat (which are not visible) raised the risk for several cancers, while subcutaneous and lower-body fat (which are visible) showed a complex, sometimes protective, relationship with cancer risk.
Subcutaneous fat was linked to a 1.8 times higher risk of endometrial cancer and a 2.3 times greater risk of esophageal adenocarcinoma, a cancer that develops in the glandular cells of the esophagus.
The UK findings align with recent research, including a 2024 American Cancer Society study linking high visceral fat scores to significantly elevated cancer risks.
Weight gain around the middle typically indicates an increase in visceral fat, a type of fat that surrounds the internal organs.
The ACS research found the most dramatic increases were for endometrial cancer, which more than doubled, and gallbladder cancer, which saw an 83 percent higher risk.
ACS researchers also found substantially elevated risks were observed for kidney (39 percent higher), liver (25 percent higher), colorectal (14 percent higher), and breast (11 percent higher) cancers.
Surprisingly, subcutaneous fat was protective, lowering the risk of luminal B and triple-negative breast cancers by 46 percent and 57 percent respectively.
The danger of visceral fat extends beyond cancer; it increases the risk of heart disease even in people with normal BMI.
Deep abdominal fat (VAT) was associated with a 39 percent higher risk of kidney cancer. Fat stored within the liver itself was associated with a 309 percent higher risk of liver cancer.
An increase in fat under the skin fat (ASAT, or subcutaneous) was associated with a 46 percent lower risk of luminal B/HER2-negative-like breast cancer and a 57 percent lower risk for triple-negative or basal-like breast cancer. Deep abdominal fat was associated with a 14 percent higher risk of colorectal cancer.
A 2018 American Heart Association report found that women who carried weight around their midsection had a 10 to 20 percent higher heart attack risk than those who were heavier overall.
Visceral fat releases inflammatory compounds that promote insulin resistance, high blood pressure, and high cholesterol, all of which work together to raise the risk of heart attack and stroke.
High amounts of visceral fat, particularly in middle age, are strongly linked to a higher risk of dementia, including Alzheimer's disease, according to an international study published last year.
Higher amounts of visceral fat were linked to significant brain shrinkage, a marker of cognitive decline and dementia.
This reduction in brain volume was seen across critical regions and was most powerful in women and younger adults, with 20 to 39-year-olds facing a nearly six-fold higher risk.